First Cancer, Now This: Improving Survivorship
- By 2026 there will be over 20 million cancer survivors alive in the US. 1
- For people diagnosed with cancer, survivorship starts at the time of diagnosis; as survivorship rates increase, so does the need for comprehensive survivorship care programs.
- A diagnosis of cancer and it’s subsequent treatment often have a huge impact on sexual health, and is one of the greatest unmet needs cited by male and female survivors.2
- Across multiple data sets, incidence of sexual dysfunction in cancer survivors ranges from 30% – 100% 2
1Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 2016; 66:271.
2Desimone M, Spriggs E, Gass JS et al. Sexual dysfunction in female cancer survivors. Am J Clin Oncol 2012. Anne Katz Phd, RN Sexuality After Cancer: A Model for Male Survivors. J Sex Med 2016: 13:70 -78
Beyond “At Least You Are Alive”
Sexual health is a multidimensional construct that goes beyond intercourse to include intimacy, body image, desire, arousal, orgasm, and relationship satisfaction.
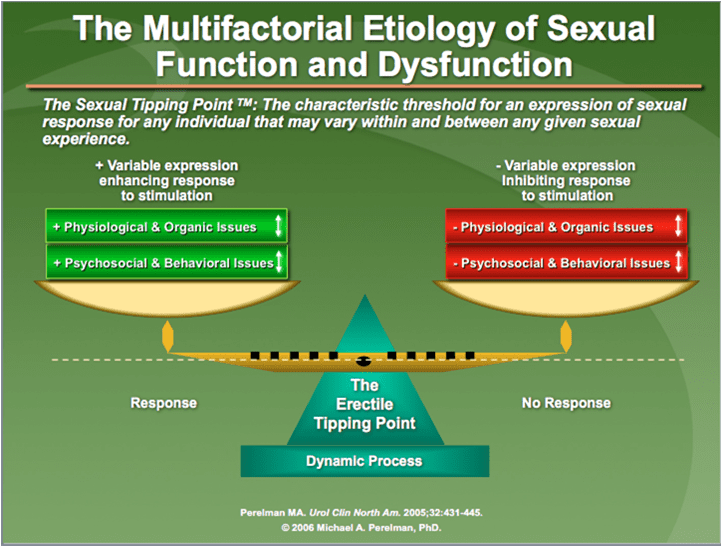
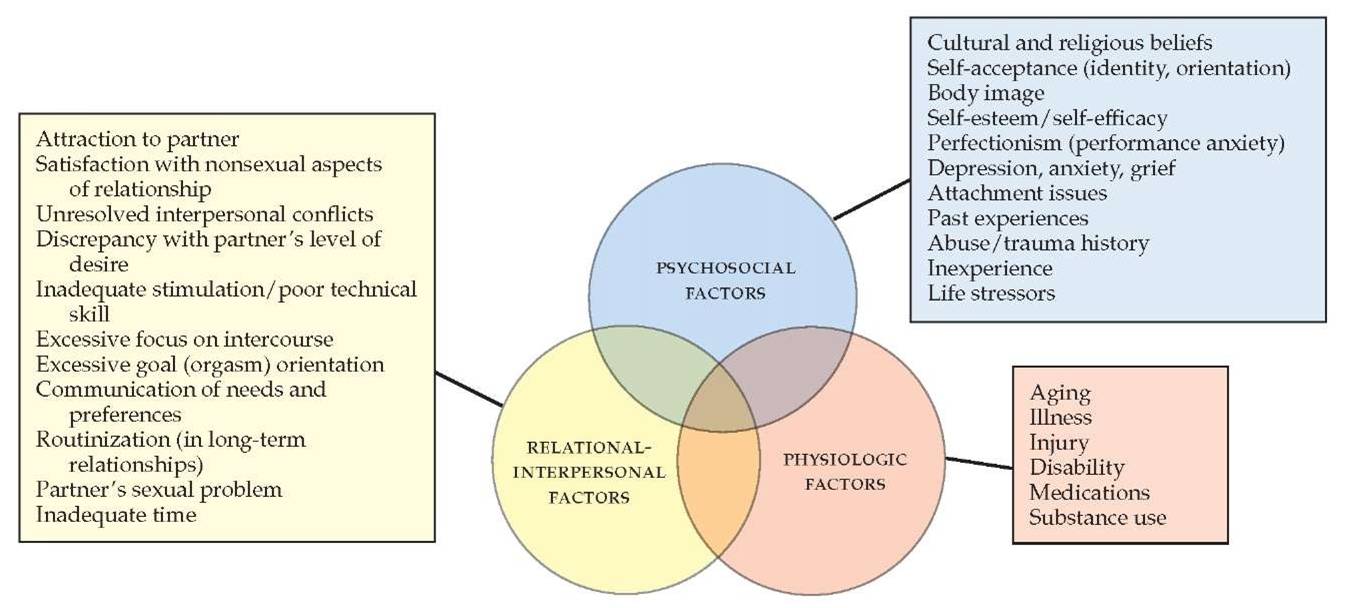
Changes in sexual function are multifactorial and complicated by issues beyond cancer and it’s treatment, further necessitating specialized care.
Common myths about sexuality after oncology care:
- Sexuality is a luxury one cannot afford in a fight for survival; just be grateful to be here
- It will get better with time or sexuality is not possible or dangerous in a diseased body
- Sex is only about penetration or orgasm; sexuality and intercourse are identical
- Sex isn’t relevant to discuss if you are single
- You are too old for sex anyway
Sexuality and Cancer: Associations and Beliefs
The Impact of Cancer on Sexual Function
| Danger | Subjectively Experienced Threat |
|---|---|
| Destruction | Destruction of Sexual Organs |
| Disfigurement | Visibly Bodily Changes |
| Handicap & Pain | Loss of Mobility, Chronic Pain |
| Dysfunction | Loss of Neurologic or Muscular Function |
| Dysregulation | Hormonal and Central Nervous Disruptions |
| Disease Load | Associated Symptoms (Incontinence, etc.) |
| Drugs | Secondary Effects |
Sexuality After Cancer
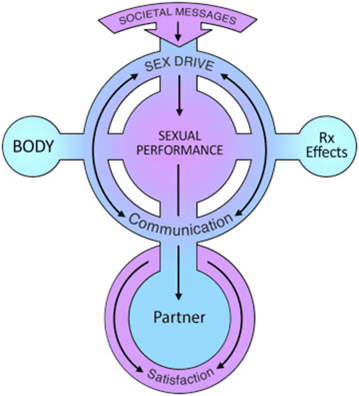
This model shows that sexual drive is influenced by societal messages, often in how “masculinity” or “femininity” is perceived and how sexual “performance” is visualized. Sexual drive is seen as being intimately associated with sexual performance, which in turn requires the contribution on the experience as viewed by the partner, who is critical in the determination of a satisfying sexual encounter.
Oncosexological Algorithm
Preexisting Personal Factors
Specific Factors of the Cancer Disease & Treatment
Invidual Response (Coping)
Clinical Syndrome of the Sexual Dysfunction
Therapeutic Objective & Treatment Plan
Biopsychosocial Model of Sexuality
Types of Sexual Dysfunctions
DSM Proposes Four Categories
Medical Care and Female Sexual Health
- Sexual dysfunction is likely to become more prevalent in breast cancer survivors with increasing use medical treatments that suppress ovarian function, and longer courses of medication that reduce hormones (aromatase inhibitors).1 (77% of breast cancer survivors report sexual problems).2
- Women need more education understanding of the safety and risks associated with hormone interventions: full body hormones are different than local vaginal hormones.
- Flibanserin (Addyi) is a medication which may be an option for women with low libido.
- Microablative C02 laser (Mona Lisa) can be appropriate treatment for women with vaginal dryness.
- Pelvic floor dysfunction can be a key cause of painful intercourse.
1National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. Survivorship. Version 1.2016. For Washington, PA: NCCN; 2016.
2Raggio GA, Butryn ML, Arigo D, et al. Prevalence and correlates of sexual morbitdity in long-term breast cancer survivors. Psychol Health 2014;29:632-650.
Medical Care and Male Sexual Health
- Men with erectile concerns after cancer should be evaluated for pre-existing causes of ED such as heart disease, diabetes, and testosterone evaluation (morning draw and repeat testing).
- Oral erectile medications, as well as penile injection therapy, penile vacuum and constriction devices, and penile implant surgery are all excellent options for men to revive sexual function.
- Early evaluation of ED following surgical recovery is optimal because untreated dysfunction may lead to permanent problems with erections due to poor oxygenation of the penis tissues.
- Men can have pelvic floor dysfunction contributing to sexual problems.
What is an Oncosexological Care Program?
- Define Sexual Health: State of physical, emotional, mental and social well being in relationship to sexuality (WHO, 2006)
- Review normal sexual response cycles, effects of menopause and aging
- Discuss sexual side effects of cancer and treatment: including biological, psychosocial and relational effects
- Review prevalence and long-term nature of cancer-related sexual issues
- Discuss classifications of sexual dysfunction
- Define Couples Sexual Health: Conceptualized as a combination of both emotional and physical connection, not performance-driven
- Review current multidisciplinary recommendations for providing cancer-related sexual health care
In Conclusion
- Sexuality is a critical quality of life issue in cancer survivorship for men and women.
- Maintaining an integrative perspective, initiating dialogue about sexual function and offering the appropriate intervention as needed can be life altering for cancer survivors.
- Modest interventions are often misunderstood or overlooked yet such strategies often have enormous potential benefit.
- Given the multiple challenges that face so many cancer survivors, it is unfortunate that too many people suffer from sexual dysfunction because they are not aware of available solutions.

Learn More About Thrive Onward
"*" indicates required fields